Bladder weakness, also known as urinary incontinence, is a common issue many women experience during menopause.
Regardless of age, bladder weakness is more common than you might think, let's talk about symptoms, causes and how to manage these annoying leaks.
As if the mood swings, hot flushes and night sweats are not enough to contend with, around *34% of adult women in the UK are affected by urinary incontinence to some degree, and many of these women are of menopausal, or peri-menopausal age.
Bladder weakness is characterised by the involuntary loss of urine. However, the symptoms vary from person to person. To identify if you are experiencing bladder weakness, you should pay careful attention to the symptoms below:
If you are experiencing any of these symptoms, it may be helpful to keep a bladder diary to track how many times you head to the toilet in a day and how much urine is produced. For convenience, you can simply take note of this on your mobile phone. The diary will assist healthcare providers to rule out any underlying medical conditions and suggest treatment options.
Well we just knew hormones would have a part to play in this, and as with so many changes during this time a decrease in oestrogen can be one of the main contributors to bladder weakness. This hormone plays a significant role in maintaining the health and strength of the tissues in the pelvic area, which yes you guessed it include the bladder and urethra! Decreasing levels of oestrogen can lead to the thinning and weakening of these tissues, making it harder for the bladder and urethra to control urine effectively.
As women age, reduced levels of oestrogen can lead to a decrease in muscle mass, tone and strength, the condition is called Sarcopenia, it can impact not only your overall muscle tone, but in many instances the muscles of the pelvic floor that support the bladder, uterus, and bowel can weaken. This weakening can result in less support for the bladder and urethra, making it more difficult to control urination. It’s one of the reasons why women over 45 are encouraged to engage in resistance and strength training, rather than continue with high activity exercises.
It's also true that as much as we love our family, childbirth may already have caused some degree of pelvic floor weakness, this combined with the effects of menopause, can exacerbate bladder control issues.
Just like other areas of the body the bladder itself may become less elastic as we age, and its capacity to hold urine may decrease, this will almost certainly lead to more frequent trips to the loo! And we can't say this enough, take as many trips as you need, don't hold it in, as this can lead to infections.
The bladder can also become more sensitive, meaning that even a small amount of urine can trigger the sensation of needing to urinate urgently.
We all love our daily caffeine hit, but did you know that caffeine, alcohol, fizzy drinks, and even certain foods like peppers and hot sauces can irritate the bladder and increase the likelihood of incontinence. That’s why keeping a diary of foods you eat for a couple of weeks, may be able to help you identify any triggers to frequent urination.

During menopause and related to hormonal shifts, bladder infections become more common during this time, and those weakened pelvic floor muscles we’ve been talking about can contribute to incomplete emptying of the bladder when you visit the toilet. This residual urine left in the bladder can then become a breeding ground for bacteria resulting in uncomfortable UTI’s.
Tips to Reduce the Risk of Bladder Infections During Menopause:
With so many causes of frequent or recurrent bladder infections during menopause, it’s a good idea to consult your doctor for more personalised advice and treatment.
Many women experience weight gain during menopause, with this extra weight being noticed particularly in the abdominal area.
This can put unexpected pressure on the bladder contributing to stress incontinence, when coughing, sneezing or laughing can result in anything from a few drips and dribbles to significant urine loss.
Being overweight can sometimes affect the nerves that sense when the bladder is full. This can lead to a condition known as overactive bladder, where there is a frequent and urgent need to urinate. If the bladder is unable to hold urine effectively due to muscle weakness or nerve issues, leaks may occur.
Mild Leakage: This could be just a few drops of urine when you cough, sneeze, laugh, or engage in physical activity.
Moderate Leakage: This might involve losing a small amount of urine (like a tablespoon or two) when pressure is exerted on the bladder.
Severe Leakage: In more severe cases, a larger amount of urine may be lost, enough to require a pad or change of clothes.
This is just a guide as the amount of urine leakage can vary significantly from person to person.
Chronic Conditions: Conditions such as diabetes, which can be more prevalent with age, can affect nerve function, including the nerves that control the bladder, leading to incontinence
The best treatment for bladder weakness varies depending on the individual and the underlying cause of their incontinence. For example, pelvic floor muscle exercises might be effective for light bladder leaks caused by stress incontinence, urge incontinence, or overflow incontinence.
It’s important to consult a healthcare professional for medical advice and to determine the best course of treatment. They’ll typically recommend a combination of treatments or refer you to a specialist for further evaluation. Urologists and physiotherapists are commonly involved in the management of bladder leaks.
It may be tempting to manage bladder weakness by limiting your water consumption, but this is certainly not a good idea. Make sure you’re drinking plenty of hydrating fluids to maintain your bladder’s capacity and stay healthy.
Bladder control exercises, also known as pelvic floor exercises, are a great way to help strengthen the bladder muscles. As we know, general exercise is so important for physical and mental well-being, so why is this any different when it comes to your pelvic floor? Strengthening this part of your body can really improve any bladder weakness you may be experiencing! These exercises are easy to do and can be done in the privacy of your own home. Before getting started, make sure you've gone to the loo and you’re in some comfy workout clothing (even an oversized shirt and leggings will do).
These exercises work by strengthening the pelvic floor muscles, helping to reduce the chances of bladder leaks. By doing these exercises regularly, you can improve your bladder control and reduce the frequency of leaking urine. There’s also the added bonus of improving your overall health and mobility through physical activity. You can take control of your bladder and your body in just a few weeks. After 4 to 6 weeks, you should start to notice improvements.

In a series of polls carried out by YouGov in 2018, it was discovered that ** a third of people believe that urinary incontinence only affects elderly women. But the reality is that it does occur amongst young adults too, typically in the form of light drips and dribbles. We simply need to create safe spaces to talk about bladder weakness more openly and ensure that people understand how to manage and treat the condition.
Another 2018 YouGov poll revealed that only ***10% of women had openly discussed their incontinence with a friend or family member. For us, the goal is to start the conversation and encourage others to do the same in their circles. This way, people will feel comfortable seeking out the products and treatments they need.
Long story short, bladder leaks are super common and can be manageable. You can still enjoy a wonderfully fulfilling life with the condition.
But let's be real, no matter how much we prepare ourselves, sometimes our bladders just have a mind of their own. That’s why it helps to have your bladder weakness diagnosed by a healthcare professional and start an effective treatment programme to get you on the right track.
From pelvic floor exercises to cutting out alcohol, there are so many options to try.
In the meantime, Lil-Lets has your back with our Extra Protection Range, including our absorbent and comfortable extra protection liners, which are ideal for light bladder leaks.
Lil-Lets Extra Protection SmartFit Liners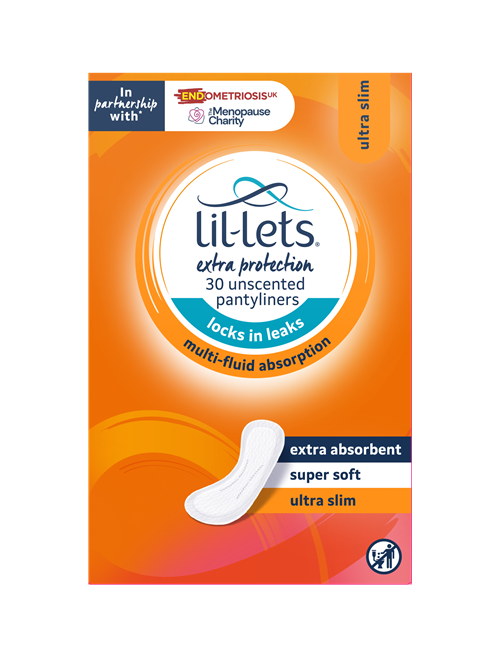
*https://www.england.nhs.uk/wp-content/uploads/2018/07/excellence-in-continence-care.pdf [Accessed: 1 February 2023]
***https://utswmed.org/medblog/leakage-
***https://www.independent.co.uk/news/health/womens-incontinence-myths-stigma-b1868540.html [Accessed: 25 January 2023]
Hormone Replacement Therapy (HRT) can potentially help with bladder weakness. The tablets have oestrogen which can strengthen the bladder and urethral muscle tissues.
Some common causes of bladder leakage include irritation, urinary tract infections (UTIs), vaginal infections, pregnancy, constipation or vigorous exercise. But no matter the cause, you probably also have weak pelvic muscles that could be strengthened.
In some cases, bladder leakage can cause a UTI (urinary tract infection) or increase the risk of bladder problems.
Bladder leakage can start at any age — it all depends on the cause. However, it’s more common among pregnant people and women over the age of 50.
Kegel exercises can certainly help with bladder leakage as they effectively strengthen the pelvic floor muscles. However, you must be consistent to see results — Kegels aren’t a quick fix!